Tuberculosis
Tuberculosis (TB), or, as it was known in the days of old,
consumption, has plagued us since before recorded history. One of the top three infectious diseases, up there with HIV/AIDS and malaria, it infects nearly a third of the world's population and still kills well over two million people yearly, largely in impoverished countries.
It's spread by inhaling fine droplets (aerosols) coughed out by an infected carrier, but accidental ingestion of a victim's mucous secretions or bodily wastes can also transmit the disease.
Complicating matters further, numerous studies have described the isolation of multi-drug resistant strains, largely due to patients not following their treatments through to completion. Make no mistake, even though it's largely out of the public eye in most of the industrialized western world, it's still very serious business.
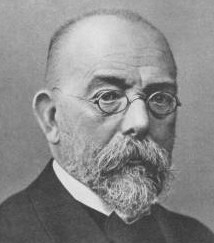
In 1882, a few years after he discovered the bacillus responsible for anthrax, German physician Robert Koch (1843-1910, at right) published his studies revealing the organism behind TB, Mycobacterium tuberculosis. Suddenly, contaminated raw milk, and it's role in infant mortality, became a lot clearer.
Just four years prior to winning the Nobel Prize in 1905, Koch reported finding that another strain, M. bovis, was responsible for tuberculosis in cows, and that it was species specific. In other words, he believed that the cow strain would not infect humans.
That belief sparked a controversy that raged until relatively recently, but still smolders unhappily today. With the completion of genome sequencing of M. tuberculosis in 1998, and M. bovis in 2003, possible new answers to old questions began to emerge.
So, can M. bovis infect people? Numerous studies show that it is, indeed, a potential zoonosis,- a fancy name for an infectious agent that normally occurs in animals (zoo-), but can cause disease (-nosis) in humans as well. Yet even with all the fingers pointing at it, many scientists refuse to believe M. bovis can infect human hosts.
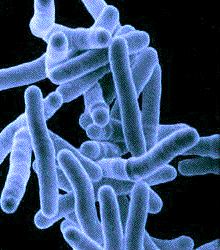
Rod shaped, slow growing and virtually identical to M. tuberculosis, (below, right), it was just about impossible to distinguish one strain from another prior to genetic analysis. Luckily, here in the U.S., where an infected animal eradication program has been in effect since 1917, chances are slim to none of contracting the disease.
Still, though almost completely eliminated from herds here in America, the possibility of re-contamination from wild animal populations (disease reservoirs) remains a concern (the white tail deer population in Michigan, brushy-tailed possums in New Zealand, to name a few), so monitoring continues, but at a much less frequent rate.
In poorer areas of the world without protective herd culling measures in place, or where large portions of the populace suffer from immune system compromising diseases like AIDS, the transmission of M. bovis from animals to humans is said to occur, but in relatively low numbers.
One interesting discovery, after unveiling the genomes of both bacterial villains, which share 99.95% identical gene sequences by the way, was that M. bovis mutated/evolved from M. tuberculosis, and not the other way around, as was widely believed.
This means that early pastoral animal tenders likely infected their cows 10-15,000 years ago, rather than having been infected by them. Knowing this, it's not too big a stretch to see how M. bovis could, over the years, again develop the potential ability to infect us. Nor is it difficult, knowing how similar these organisms are, to see how easily one could be mistaken for the other in attempting to determine the causative agent in a disease.
Whether the bulk of tuberculosis traceable to raw milk in earlier times was the result of external contamination (unsanitary conditions; infected, tubercular workers) or lesions in the udders of cows racked with bovine tuberculosis, it's difficult to say.
Remember that before the advent of mechanical milking systems in the 1920's, milk exiting the udder was exposed to the air and any contaminants it contained.
The milk buckets, too, were easily contaminated. A tubercular worker hacking into even one bucket could contaminate thousands of gallons when his milk was poured into a larger batch.
Today, vacuum hoses gently remove the milk from sanitized teats, completely shielding it from exposure to the environment and any possible pathogenic organisms that might be blowing about.
Cows, raised on pasture, rather than confined to manure laden enclosures, have much less exposure to disease-causing, feces-dwelling organisms (plus sunlight destroys M. bovis) and thus enjoy the added benefit of being healthier overall.
On top of all that, the historical record is full of cultures from all over the world who subsisted on raw dairy products, with no refrigeration, no processing, and most importantly, no tuberculosis. Choose your raw milk source carefully and you'll be able to say the same.
For an excellent account of the whole raw milk/tuberculosis issue, see Dr. Ron Schmid's book, The Untold Story of Milk, available in our Selected Books section.